Care coordination, which is the deliberate organization of patient care activities across multiple participants, is undergoing a profound technological transformation. Driven by the shift to value-based care, digital innovations are breaking down traditional silos and creating interconnected health ecosystems focused on enhancing patient outcomes, reducing costs, and improving efficiency. This third installment in a five-part series on the valuation of care coordination services reviews the technology supporting, augmenting, and advancing care coordination services.
Integrated Data and Interoperability
The foundation of modern care coordination is the seamless, secure exchange of patient information across different systems, providers, and settings. For example, electronic health records (EHR) remain a foundational technology, providing a centralized, digital version of a patient’s medical record. Their utility has advanced beyond simple documentation to become central hubs for sharing and storing patient data.1 Patient portals provide patients direct access to both their health information and clinicians, supporting care coordination by allowing them to actively participate in their care.2 Historically, healthcare information technology (HIT), such as those described above, was utilized in silos and were not integrated. More recently, however, digital health companies have sought to combine these various applications, and add new functions and applications, revolutionizing care coordination through HIT.3
Care Coordination Software
Care coordination software, also referred to as care coordination information technology (CCIT), which refers to software applications designed to enable various functions related to managing the care of a provider’s patients, has been the focus of many digital healthcare companies, with the U.S. care coordination software market expected to grow to $3.18 billion by 2022 (up from $1.55 billion in 2019).4 The components and capabilities of such software vary widely, but may perform such tasks as automating referral management; communication to a patient’s care team (e.g., automated email updates to patient status and patient hospital admission/discharge); delivery of discharge instructions and next steps to a patient’s primary care provider; and, reports that provide real-time utilization trends, outreach success rates, and no-show rates.5 These technologies are also being aided by artificial intelligence and blockchain technology, “which support data interoperability and normalization within a defined clinical network.”6 Among other capabilities, these technologies allow for constant, two-way communication among providers in the acute, post-acute, and primary care spaces; this is significant as communication (or lack thereof) among providers in these spaces tends to be the root of many care coordination issues.
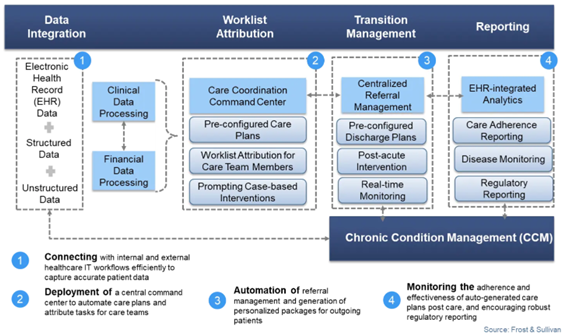
The below exhibit illustrates how care coordination workflow may ideally work with the use of technology.
The technologies described above, as well as other data analytics, will be needed by participants in value-based reimbursement models, which typically rely on pre-established benchmarks and require participants to report on patient outcomes.8
Despite the potential benefits of HIT and care coordination software, adoption of these technologies poses significant administrative and cost burdens to small providers.9
Artificial Intelligence (AI)
AI is becoming an increasingly essential element for modern care coordination. Some of its most popular applications include:
-
Predictive risk stratification: AI and machine learning analyze big datasets to identify high-risk patients who may benefit from early, proactive intervention. For example, algorithms can predict patients who are at a high risk for hospital readmission, allowing care teams to intervene with preventative measures.
-
Workflow automation: AI automates routine, administrative tasks, such as creating clinical summaries, prioritizing tasks, and managing patient discharge planning, which reduces the administrative burden on clinicians, freeing them to focus on patient care.
-
Clinical decision support: AI augments clinical decision-making by analyzing patient data, enhancing care plans, and providing actionable insights and evidence-based recommendations at the point of care.10
While there remain privacy, security, and ethical concerns surrounding the use of AI, its use can drive cost savings and enhance revenue streams for healthcare organizations by automating administrative tasks, improving diagnostic accuracy, enabling proactive interventions.11 In the future, AI’s role will likely become even more sophisticated and integrated, creating a robust, intelligent ecosystem that promises not only to improve patient care, but to transform the economic and operational landscape of healthcare.
Telehealth
Telehealth is revolutionizing care coordination by; breaking down geographical barriers, enhancing communication, and enabling continuous patient monitoring. Specialists can remotely consult, promoting timely diagnoses and treatment decisions. As noted by one source:
“[r]esearch has shown that effective care coordination allows for earlier detection of problems, more precise intervention, and increased patient confidence in providers. When utilized properly, virtual care [such as telehealth] advances care coordination because it allows for
-
Fewer unreimbursed hospital readmissions,
-
Improved capture of wellness screenings,
-
Optimization of value-based indicators, such as timeliness of appointments and prompt answering of care-related questions, and
-
New sources of revenue previously untapped through reimbursement for activities formerly considered to be simply the ‘work of the day.’”12
Notably, remote patient monitoring (RPM) — “the use of digital devices to monitor a patient’s health”13 — is becoming a more critical component of telehealth that elevates care coordination beyond episodic visits to continuous, proactive management. For example, “with post-hospital discharge, telehealth enables remote monitoring of vital signs, allowing healthcare providers to track patients’ progress, identify potential complications early on and reduce readmissions. This proactive approach minimizes the risk of readmissions and improves patient outcomes.”14 As RPM continues to evolve, it stands to significantly advance care coordination by enabling continuous oversight, early intervention, and improved patient outcomes throughout the continuum of care.
Conclusion
As one study noted, “Innovative care coordination solutions depend on a modern data platform strategy.”15 HIT, AI, and telehealth are rapidly redefining the landscape of healthcare by streamlining operations, enhancing care quality, and offering new opportunities for patient engagement. As these technologies continue to mature and integrate more deeply into clinical workflows, healthcare organizations are poised to achieve greater efficiency, improved outcomes, and stronger financial sustainability. Embracing these innovations will be essential for providers who seek to remain competitive and responsive to the evolving needs of patients and the broader healthcare system.
The next installment in this five-part series will explore the reimbursement environment in which care coordination services are provided.
“What Is Care Coordination in Healthcare and Why Is It Important?” Care Coordinations, July 10, 2024, https://carecoordinations.com/blog/what-is-care-coordination-in-healthcare-and-why-is-it-important (Accessed 10/23/25).
“Lumeon wins big in Frost & Sullivan’s latest research on the US Care Coordination Market” Frost & Sullivan, https://www.frost.com/frost-perspectives/lumeon-wins-big-in-frost-sullivans-latest-research-on-the-us-care-coordination-market/ (Accessed 10/23/25).
Ibid; “AI-powered Care Coordination Software Gives Vendors Competitive Edge in the Era of Personalized Healthcare” By Mariana Fernandez, Frost & Sullivan, April 10, 2019, https://www.frost.com/news/press-releases/ai-powered-care-coordination-software-gives-vendors-competitive-edge-in-the-era-of-personalized-healthcare/ (Accessed 10/23/25).
“Care Management: It’s More than Population Health” By Greg Caressi & Kustav Chatterjee, Frost & Sullivan, 2017, available at: https://www.experian.com/content/dam/marketing/na/healthcare/white-papers/frost-sullivan-care-management-population-health-outcomes.pdf (Accessed 10/23/25), p. 4.
Frost & Sullivan, Press Release, April 10, 2019.
“Lumeon wins big in Frost & Sullivan’s latest research on the US Care Coordination Market” Frost & Sullivan, https://www.frost.com/frost-perspectives/lumeon-wins-big-in-frost-sullivans-latest-research-on-the-us-care-coordination-market/ (Accessed 10/23/25).
“Medical Case Management Services in the US” By Marley Brocker, IBISWorld, Industry Report OD5774, August 2025, p. 14.
“EHRs: The Challenge of Making Electronic Data Usable and Interoperable” By Miriam Reisman, P&T, Vol. 42, No. 9 (September 2017), available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5565131/pdf/ptj4209572.pdf (Accessed 10/23/25), p. 574; “Do Small Physician Practices Have a Future?” By David Squires and David Blumenthal, M.D., To The Point, The Commonwealth Fund, May 26, 2016, https://www.commonwealthfund.org/blog/2016/do-small-physician-practices-have-future (Accessed 10/23/25).
“Improve Care Coordination and Delivery with AI & HealthEdge GuidingCare®” By Allison Peterson, HealthEdge, June 10, 2025, https://healthedge.com/resources/blog/gc-improve-care-coordination-and-delivery-with-ai-healthedge-guidingcare (Accessed 10/23/25).
“Aidoc's AI Care Coordination Platform: A New Era for Hospital Domains” By Ayden Jacob, MD, MSc and Demetri Giannikopoulos, Aidoc, January 30, 2025, https://www.aidoc.com/learn/blog/ai-care-coordination-platform/ (Accessed 10/23/25).
“Leveraging telemedicine to improve care coordination and financial recovery” By Shelly Turner, DNP, MBA, BS, CPHQ, Press Ganey, February 1, 2021, https://info.pressganey.com/press-ganey-blog-healthcare-experience-insights/leveraging-telemedicine-to-improve-care-coordination-and-financial-recovery (Accessed 10/23/25).
“Telehealth and Remote Patient Monitoring” Telehealth.HHS.gov, last updated August 28, 2024, https://telehealth.hhs.gov/providers/best-practice-guides/telehealth-and-remote-patient-monitoring#:~:text=Remote%20patient%20monitoring%20is%20the,and%20provider%2C%20and%20patient%20engagement. (Accessed 10/23/25).
Clement, OpenLoop, May 25, 2023.
“IDC MarketScape: U.S. Care Coordination Technology: 2024–2025 Vendor Assessment” By Jennifer Eaton, IDC MarketScape, available at: https://healthedge.com/resources/executive-summaries/idc-marketscape-u-s-care-coordination-technology-2024-2025-vendor-assessment (Accessed 10/23/25), p. 3.