As discussed in the first installment of this five-part series regarding Rural Health Clinics (RHCs), the significant proportion of RHCs operating at a loss has led to an overall reduction in the number of RHCs.1 Despite this decrease, the demand for RHCs continues to rise, limiting access to care for patients in rural communities.2 This second installment will review the competitive environment of RHCs.
Supply of RHCs
As of July 2018, there were approximately 4,300 RHCs across the U.S.3 However, the number of RHC closures is rising, with 98 closures from 2010 to February 2019, and approximately 46% of active RHCs operating at a loss (potentially signaling additional closures in the future).4 These financial issues typically stem from the disproportionate number of Medicare and Medicaid patients (i.e., patients whose insurance coverage reimburses providers less than commercial insurance) that utilize RHCs.5 As of 2018, there were 7,026 primary care Health Professional Shortage Areas (HPSAs) in the U.S., with 59% of those HPSAs located in rural areas.6 These statistics indicate an insufficient supply of healthcare organizations such as RHCs for the size of the U.S. population living in rural areas.
Additionally, the overall supply of rural health services is expected to decrease as the number of physicians (especially primary care providers) decrease, with more physicians currently moving toward retirement than the number of residents entering the profession.7 Further, the primary care physician to patient ratio is 39.8 physicians per 100,000 people in rural areas, compared to 53.3 physicians in urban areas.8 Due to a lack of primary care physicians entering the field, and the current limited number of primary care physicians practicing in rural areas, the supply of rural health services could further decrease in the future.
Demand Drivers of RHCs
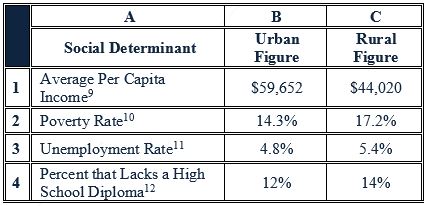
The demand for rural health services is driven by various social and health determinants, as well as by the proximity of a patient to an RHC. As set forth below in Table 1, the rate of various social determinants of health are more acute in the rural areas of the U.S. than in the urban areas, potentially indicating a less healthy population (and thus greater need for healthcare services) in rural locations.
Table 1: Social Determinant Comparisons between Urban/Rural Areas
In addition to these social determinants, a number of health determinants, such as smoking and obesity, drive demand for rural health services. Across the U.S., those who live in rural areas have higher rates of smoking and smokeless tobacco utilization, as well as an earlier age at which smoking habits develop.13 Smoking increases the risk of coronary heart disease, stroke, and lung cancer, and diminishes the overall health of an individual, contributing to the increased demand for healthcare resources.14 Not only do more rural residents smoke than urban residents, they also smoke more frequently – those that live in rural areas are more likely to smoke more than 15 cigarettes a day, compared to those in urban areas, who are more likely to smoke six or fewer cigarettes a day.15
In addition to an increased demand for healthcare services, driven in part by the smoking habits of adults in rural areas where RHCs are located, a large number of Americans are considered obese. Approximately 39.6% of U.S. adults are obese (i.e., reported a body mass index ≥ 30).16 Additionally, a majority of adults are physically inactive, with only 51.7% of adults meeting the national Physical Activity Guidelines for aerobic activity.17 In turn, obesity, which has a greater prevalence among rural adults, contributes to increased chronic conditions and higher utilization of medical services, leading to increased demand for rural health services, driven by complications due to obesity.18 In addition, obesity rates are higher among rural children and adolescents than in urban children, with rural children having 26% greater odds of becoming obese compared to urban children.19 Studies have also shown that rural children engage in less physical activity compared to urban children, in which physical activity barriers include: isolation; lack of transportation; climate and terrain; safety concerns; and, lack of access to locations with physical activity opportunities.20 Further, overweight children are more prone to become overweight adults, exacerbating this health determinant within rural areas.21 The high rate of obesity in adults and children, as well as the contributing factor of physical inactivity, effectively increases healthcare demand by the rural patient population.
However, according the U.S. Department of Agriculture (USDA), population growth rates have been significantly lower in rural counties than in urban counties.22 Many communities have experienced a net population loss, with a majority of the Northeast and Midwest rural counties losing population since the 2000s.23 Many of those individuals leaving rural communities are younger, causing the median age in rural communities to rise, exacerbating the age difference compared to urban or suburban areas.24 Additionally, the older population is expected to rise significantly as the Baby Boomer cohort ages, causing the number of older adults to increase by 18 million by 2030.25 With the increase in the elderly population in rural communities (who will inevitably utilize a disproportionate amount of care), demand for RHCs will continue to rise despite the rural population out-migration.
Future Outlook
Despite current instability in the RHC market, as well as in rural healthcare generally, the Centers for Medicaid and Medicaid Services (CMS) is taking steps to implement new policies that will positively impact rural healthcare. On September 20, 2018, CMS released a proposed rule to reduce unnecessary regulatory burdens within the Medicare program, including several proposals to reduce burdens for RHCs.26 Reduced regulatory burden may increase the ease of entry into the rural health market or improve the financial status of RHCs, potentially increasing the supply of RHCs in the future. Additionally, the RHC Modernization Act, introduced by Senators John Barrasso (R-WY) and Tina Smith (D-MN), aims to ensure that people in rural areas have access to healthcare services, as there is still a shortage of providers.27 Because many RHCs are heavily dependent on Medicare and Medicaid reimbursement, the Act proposes to increase the RHC all-inclusive rate (AIR), i.e., the fixed reimbursement for all RHC visits.28 An increase to reimbursement could potentially help the 43% of RHCs that are operating at a loss and are at risk for closure.29 Additionally, an increase in reimbursement could draw more physicians into rural areas, as well as loan forgiveness and repayment options available to physicians practicing in Health Professional Shortage Areas (HPSAs).30 Additionally, non-physician providers (NPPs), such as nurse practitioners (NPs) or physician assistants (PAs), often have extended scope of practice, which can range from autonomous practice to direct physician oversight depending on state regulations.31 Increased reimbursement, as well as options for loan forgiveness and repayment programs, may draw NPPs to rural communities.32
The increase in demand for rural healthcare services is expected to increase due to the aging Baby Boomer population and the overall unhealthiness of rural communities, due to both social determinants, e.g., the relatively high unemployment and poverty rates, and health determinants, e.g., higher rates of smoking and obesity rates, in those areas.33 However, the decrease in supply of RHCs and primary care providers results in a critical shortage of rural health services that are wholly insufficient to meet the rising demand. The next installment of this series will examine the reimbursement environment of RHCs.
“Valuation of Rural Health Clinics: Introduction” Health Capital Topics, Vol. 12, Issue 3 (March 2019), available at: https://www.healthcapital.com/hcc/newsletter/03_19/HTML/CLINIC/convert_hc_topics_rhc_intro_3.27.19a.php
“Demographic Changes and Aging Population” Rural Health Information Hub, https://www.ruralhealthinfo.org/toolkits/aging/1/demographics (Accessed 4/10/19).
“United States: Rural Healthcare Facilities” Rural Health Information Hub, https://www.ruralhealthinfo.org/states/united-states (Accessed 3/7/19).
“Rural Hospital Closures to Ninety-Eight” By Jessica Seigel, National Rural Health Association, February 20, 2019, https://www.ruralhealthweb.org/blogs/ruralhealthvoices/february-2019/rural-hospital-closures-rise-to-ninety-seven (Accessed 3/7/19).
“Verma’s promise to rural providers: You come first” By Susannah Luthi, Modern Healthcare, February 6, 2018, https://www.modernhealthcare.com/article/20180206/NEWS/180209939/verma-s-promise-to-rural-providers-you-come-first (Accessed 4/10/19).
First Quarter of Fiscal Year 2019 Designated HPSA Quarterly Summary” Bureau of Health Workforce, Health Resources and Services Administration (HRSA), U.S. Department of Health & Human Services (January 1, 2019), p. 3.
“The Complexities of Physician Supply and Demand: Projections from 2016 to 2030” Submitted by IHS Markit Limited, for the Association of American Medical Colleges, March 2018, https://aamc-black.global.ssl.fastly.net/production/media/filer_public/85/d7/85d7b689-f417-4ef0-97fb-ecc129836829/aamc_2018_workforce_projections_update_april_11_2018.pdf (Accessed 12/28/18).
“Rural Providers Need New Strategies to Succeed” By Erin Hennessey, MA, NHA, CPG, Provider Magazine, December 2018, http://www.providermagazine.com/archives/2018_Archives/Pages/1218/Rural-Providers-Need-New-Strategies-to-Succeed.aspx (Accessed 4/10/19).
“Poverty Rates/Median Household Income in United States by County Type: 2013-2017” United States Census Bureau, https://www.census.gov/library/visualizations/2018/comm/acs-5yr-poverty-type.html (Accessed 4/10/19).
“Rural Employment and Unemployment” United States Department of Agriculture, Economic Research Service, 2017, https://www.ers.usda.gov/topics/rural-economy-population/employment-education/rural-employment-and-unemployment/ (Accessed 4/10/19).
“Rural education levels are increasing, but still lag behind urban areas” By Economic Research Service, 2018, https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=90366 (Accessed 4/10/19).
“Tobacco Use in Rural Areas” Rural Health Information Hub, https://www.ruralhealthinfo.org/toolkits/tobacco/1/use-in-rural (Accessed 3/7/19).
“Health Effects of Cigarette Smoking” Centers for Disease Control and Prevention, May 15, 2017, https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm (Accessed 12/17/18).
Rural Health Information Hub, 2018; “Cutting Tobacco’s Rural Roots: Tobacco Use in Rural Communities” American Lung Association, 2010, https://www.lung.org/assets/documents/research/cutting-tobaccos-rural-roots.pdf (Accessed 4/11/19), p. 6.
The seven states include: Alabama, Arkansas, Iowa, Louisiana, Mississippi, Oklahoma, and West Virginia. “New Report Shows U.S. Obesity Epidemic Continues to Worsen” By Michal Devitt, AAFP, October 15, 2018, https://www.aafp.org/news/health-of-the-public/20181015obesityrpt.html (Accessed 3/7/19).
“Physical Inactivity in the United States” The State of Obesity, September 2018, https://www.stateofobesity.org/physical-inactivity/ (Accessed 3/7/19).
“Prevalence of Obesity Among Adults from Rural and Urban Areas of the United States: Findings From NHANES (2005-2008)” By, Christie Befort, Niaman Nazir, and Michael Perri, Journal of Rural Health, Vol. 28, No. 4, (May 31, 2012), p. 1; “The Impact of Obesity on Health Care Utilization and Expenditures in a Medicare Supplement Population” By Shirley Musich, et al., Gerontology & Geriatric Medicine, (January 19, 2016), p. 1.
“Urban-Rural Differences in Childhood and Adolescent Obesity in the United States: A Systematic Review and Meta-Analysis” By James Allen Johnson III, and Asal Mohamadi Johnson, Vol. 11, No. 3 (June 2, 2015), p. 1.
“Promoting Active Living in Rural Communities” Active Living Research, September 215, https://activelivingresearch.org/sites/activelivingresearch.sdsc.edu/files/ALR_Brief_RuralCommunities_Sept2015.pdf (Accessed 4/11/19).
“Childhood obesity and adult morbidities” By Frank M. Biro and Michelle Wien, The American Journal of Clinical Nutrition, Vol. 91, No. 5 (2010), p. 1499S.
Hennessey, MA, NHA, CPG, December 2018.
“Demographic and economic trends in urban, and suburban and rural communities” By Kim Parket, et al., Pew Research Center, May 22, 2018, https://www.pewsocialtrends.org/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/ (Accessed 4/10/19).
“Rural America is Losing Young People – Consequences and Solutions” Wharton University of Pennslyvania, Public Policy Initiative, March 23, 2018, https://publicpolicy.wharton.upenn.edu/live/news/2393-rural-america-is-losing-young-people- (Accessed 4/4/19); “Demographic and economic trends in urban, and suburban and rural communities” By Kim Parket, et al., Pew Research Center, May 22, 2018, https://www.pewsocialtrends.org/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/ (Accessed 4/10/19).
Rural Health Information Hub, https://www.ruralhealthinfo.org/toolkits/aging/1/demographics.
“CMS Seeking to Reduce RHC Regulatory Burden” By Nathan Baugh, Director of Government Affairs, National Association of Rural Health Clinics, September 21, 2018, https://www.web.narhc.org/News/27611/CMS-Seeking-to-Reduce-RHC-Regulatory-Burden (Accessed 4/10/19).
“Rural Health Clinic Modernization Act” Nathan Baugh, Director of Government Affairs, National Association of Rural Health Clinics, April 4, 2019, https://www.web.narhc.org/News/27847/RHC-Modernization-Act-Introduced-by-Senator-Barrasso-and-Senator-Smith (Accessed 4/19/19); “Barrasso, Smith Introduce Bipartisan Rural Health Clinic Modernization Act” John Barrasso, April 3, 2019, https://www.barrasso.senate.gov/public/index.cfm/2019/4/barrasso-smith-introduce-bipartisan-rural-health-clinic-modernization-act (Accessed 4/11/19).
“Rural Hospital Closures to Ninety-Eight” By Jessica Seigel, National Rural Health Association, February 20, 2019, https://www.ruralhealthweb.org/blogs/ruralhealthvoices/february-2019/rural-hospital-closures-rise-to-ninety-seven (Accessed 3/7/19).
“Programs for Loan Repayment and Forgiveness: A List for Rural Providers” By Laura Grangaard, MPH, Rural Health Information Hub, February 12, 2014, https://www.ruralhealthinfo.org/rural-monitor/loan-repayment-and-forgiveness/ (Accessed 4/11/19).
“Impact of Nurse Practitioner Practice Regulations on Rural Population Health Outcomes” By Judith Ortiz, et al., Healthcare, Vol. 6, No. 2, (June 2018), p. 1.
Rural Health Information Hub, February 12, 2014.
“Rural Employment and Unemployment” United States Department of Agriculture, Economic Research Service, 2017, https://www.ers.usda.gov/topics/rural-economy-population/employment-education/rural-employment-and-unemployment/ (Accessed 4/10/19); “Poverty Rates/Median Household Income in United States by County Type: 2013-2017” United States Census Bureau, https://www.census.gov/library/visualizations/2018/comm/acs-5yr-poverty-type.html (Accessed 4/10/19).





